With all of the bush fires around the East Coast lately, many people have experienced the effects of smoke inhalation. So, to help people to understand what to do and what effect it has on the lungs.
To do this, it is essential to understand what is happening in our lungs, how they defend against this type of invasion and what we need to do to reduce the change of any potential short and long term damage may be.
The way in which the lungs defend themselves is the part where differences between asthma attack symptoms and respiratory attack symptoms become apparent (even though they may feel the same).
As explained in a previous article “Mystery of How Eating Causes Asthma Attacks”, the way the body reacts to different types of foreign particles is, and is explained further in the section “What is the Difference Between Normal Defense and Asthmatic Defense?”.
In the article below, I will explain what the respiratory response is to excessive smoke , the different phases and what the effects are.
Respiratory Response to Excess Smoke and Foreign Particles
Mucociliary Escalator
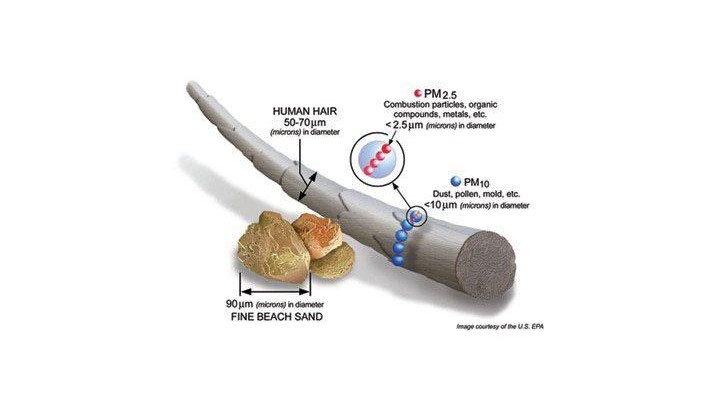
The airways have an efficient mechanism called the Mucociliary Escalatory. This includes a combination of hairs on the airway walls called cilia, which captures up to 90% of foreign particles. When a large number of particles enter the lungs, initially the mucociliary escalator works as normal and is able to clear these particles efficiently.
But as the number of particles increases and become more consistent, which is the case with medium to long term exposure to bush fire smoke, the following steps occurs.
Step 1 - Mucus becomes contaminated – The smoke starts building up in the mucus, changing colour. Over time, some of these particles may reach the airway walls, also known as the epithelium (i.e. skin cells), causing the lungs to triggers Step 2.
Step 2 – Cough - When the airway walls are agitated by the foreign particles, we have a more explosive defence mechanism called a cough. This can be either instigated manually by ourselves or as a reflex by our body.
The cough is usually employed to assist in the following:
- Assist in clearing an excess amount of airborne foreign particles comping into the lungs,
- Cause wind sheering of the top layers of the mucus, assisting in mobilising and removing new particle which have settled in the mucus,
- Assist to mobilise the mainstream of mucus - If the mucus has built and is no longer moving in an efficient manner, then the airways can become restricted and the mucociliary escalator becomes heavy and weighed down. A cough can assist to give the mucus a push start and help it to start moving more efficiently.
If the agitation of the airway walls continues and aren’t cleared, then Step 3 is triggered.
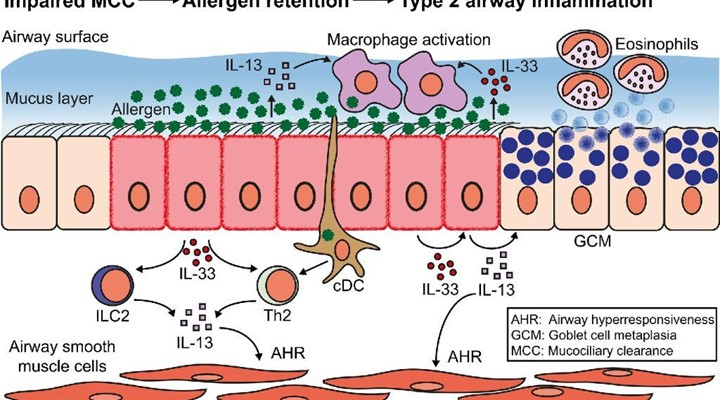
Step 3 – Immune System Response – The consistent agitation and invasion of the particles onto and into the airway walls (epithelium), causes the following 2 processes to occur:
- Hypersecretion of mucus – This is a medical term of simply saying that the mucus becomes thicker when changing its properties and the amount of mucus is increased, thus providing a thicker barrier against the foreign particles. This is an attempt to stop any further particles from reaching the airway walls and reduce agitation and/or infection,
- Inflammation of the Airway Walls – This is the way in which the airway walls help to clear the foreign particles, bacteria, etc… which have already made it through the mucus. The blood vessels of airway walls release blood into the tissue called inflammation (which causes expansion of the tissue). This allows the white blood cells, from the immune system, to attack and digest the particles, helping to clear them from the area as quickly as possible.
So what does this mean?
This means that where a healthy fire fighter may be able to have a break for at least 3 hours to assist with removal of up to 49% of the smoke particles, a fire fighter with a respiratory condition should have a break of at least 17 hours to assist with the removal of up to 42% of the smoke particles.
Issues with Long Term Exposure
If you have a long term exposure to smoke, then your lungs become filled with smoke particles and may lead to smoke particles going into the alveoli (air sacs where gas transfer occurs). This may lead to inflammation of the alveoli, which includes an immune defense of inflammation of the air sacs. This is where the blood vessels of the air sacs open up and bleeding into the alveoli, helping the white blood cells to fight and digest the smoke particles.
The other issue which may be faced in the airways is that the lungs may develop structural defects of the cilia and epithelium (skin cells). This may lead to an extended length of time for which deposited particles stay in the airways.
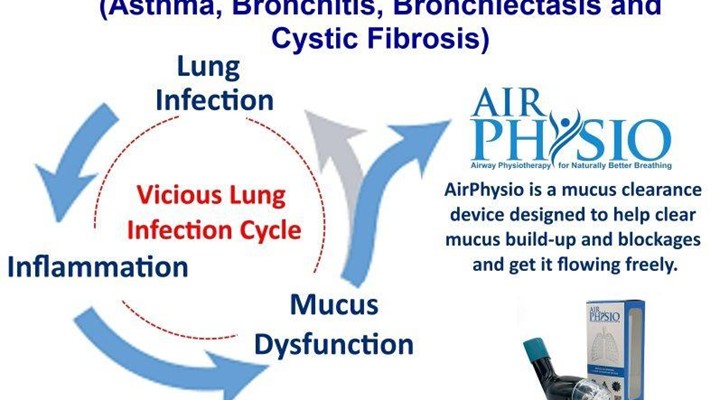
This may cause a longer period of exposure to harmful airborne particulate matter, occupational dusts, traffic exhaust and smoke. This creates a vicious cycle of events where the particles are deposited in the airways, they may cause further infection, inflammation and excess mucus to become released.
This in turn may lead to further mucus build up, causing further infection, inflammation and excess mucus to become released, and the cycle goes on. This may lead to medium to long term damage of the lungs.
What Can Be Done to Help Stop Further Damage?
Like everything, the first step is to stop the source of the problem which is causing the damage in the first place. This will help the cleaning and healing process to start by allowing the lungs to do what they need to do, i.e. to maintain optimal hygiene and repair the damage.
So to help the body to start the cleaning process, then you need to do the following:
- Give yourself a break away from the smoke of at least 3 hours health people (49% of particle matter) and over 17 hours for people with respiratory conditions (42% of particle matter),
- Drink plenty of water and electrolytes – This will help to hydrate your mucus, helping the contaminated mucus to flow easier and be cleared more efficiently,
- Use Mucus Clearance techniques and/or devices – This way you can assist the body to expel the contaminated mucus more effectively. There are many techniques and mucus clearance devices which you can use, ranging from forced coughs to pursed lip breathing techniques, through to PEP and OPEP devices which assist with mucus clearance.
- Seek medical assistance and/or advice (if required) and/or take prescription medication (if required) to assist in reducing the inflammation.
In Conclusion
The body is amazing and can cope with a number of extreme conditions, but it is important to not overexpose the lungs to an excess amount of smoke as it may lead to medium to long term damage.
The above mentioned points will assist in helping your body to cope better with the excess smoke, while helping your lungs to expel these foreign particles, excess contaminated mucus and maintain optimal lung capacity.
References
- Scheuch, G., Kohlhaufl, M., Moller, W., Brand, P., Meyer, T., Haussinger, K.,… Heyder, J. (2008). Particle clearance from the airways of subjects with bronchial hyperresponsiveness and with chronic obstructive pulmonary disease. Experimental Lung Research, 34, 531-549. doi:10.1080/01902140802341710
- Möller, W., Häußinger, K., Ziegler-Heitbrock, L., & Heyder, J. (2006). Mucociliary and long-term particle clearance in airways of patients with immotile cilia. Respiratory Research, 7(10), 1-8. doi:10.1186/1465-9921-7-10
- Brown, J. S., Zeman, K. L. & Bennett, W. D. (2002). Ultrafine particle deposition and clearance in the healthy and obstructed lung. American Journal of Respiratory and Critical Care Medicine, 166, 1240–1247. doi:10.1164/rccm.200205-399OC
- Osadnik, C.R., C.F. McDonald, B.R. Miller, C.J. Hill, B. Tarrant, R. Steward, C. Chao, N. Stodden, C.C. Oliveira, N. Gagliardi, and A.E. Holland, The effect of positive expiratory pressure (PEP) therapy on symptoms, quality of life and incidence of re-exacerbation in patients with acute exacerbations of chronic obstructive pulmonary disease: a multicentre, randomised controlled trial. Thorax, 2014. 69(2): p. 137-43.
- Forbes, L., Kapetanakis, V., Rudnicka, A., Cook, D., Bush, T., Stedman, J.,… Anderson, J. (2009). Chronic exposure to outdoor air pollution and lung function in adults. Thorax, 64, 657-663. doi:10.1136/thx.2008.109389
- Downs, S., Schindler, C., Liu, S., Keidel, D., Bayer-Oglesby, L., Brutsche, M.,… SAPALDIA Team (2007). Reduced exposure to PM10 and attenuated age-related decline in lung function. The New England Journal of Medicine, 357(23), 2338-2347. doi:10.1056/NEJMoa073625
- Morsch, A.L., Amorim, M. M., Barbieri, A., Santoro, L. L., & Fernandes, A.L. (2008). Influence of oscillating positive expiratory pressure and the forced expiratory technique on sputum cell counts and quantity of
induced sputum in patients with asthma or chronic obstructive pulmonary disease. Jornal Brasileiro De Pneumologia : Publicacao Oficial Da Sociedade Brasileira De Pneumologia E Tisilogia, 34 (12), 1026-32.