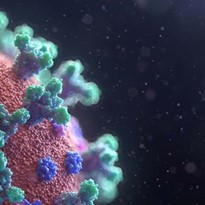
February 20, 2020 — The American College of Cardiology (ACC) released a clinical bulletin addressing the cardiac implications of the novel coronavirus (COVID-19, also referred to as SARS-CoV-2, 2019-nCoV and Wuhan Coronavirus). The key message to clinicians is that patients with underlying cardiovascular disease may have a potential increased risk if they contract coronavirus.[1]
The bulletin provides background on the epidemic, which was first reported in late December 2019, and looks at early cardiac implications from case reports. It also provides information on the potential cardiac implications from analog viral respiratory pandemics and offers early clinical guidance given current 2019-nCoV uncertainty.
Read the ACC bulletin.
In particular, the bulletin notes that “in geographies with active 2019-nCoV transmission (mainly China), it is reasonable to advise patients with underlying cardiovascular disease of the potential increased risk and to encourage additional, reasonable precautions.” It stresses the importance for cardiovascular disease patients to “remain current with vaccinations, including the pneumococcal vaccine given the increased risk of secondary bacterial infection” and suggests encouraging the “influenza vaccination to prevent another source of fever which could be initially confused with coronavirus infection.”
Watch the VIDEO: What Cardiologists Need to Know about COVID-19 — Interview with Thomas Maddox, M.D., chair of the ACC committee that created the document.
Cardiac Implications of Novel Coronavirus:
The ACC lists the following points regarding early cardiac implications from case reports on Wuhan Coronavirus.[2]
• Early case reports suggest patients with underlying conditions are at higher risk for complications or mortality from COVID-19; up to 50 percent of hospitalized patients have a chronic medical illness.
• 40 percent of hospitalized patients with confirmed COVID-19 patients have cardiovascular or cerebrovascular disease.
• In a recent case report on 138 hospitalized COVID-19 patients, 19.6 percent of patients developed acute respiratory distress syndrome.[3]
• 16.7 percent of patients developed arrhythmia; 7.2 percent developed acute cardiac injury.
• 8.7 percent of patients developed shock; 3.6% developed acute kidney injury.
• Rates of complication were universally higher for ICU patients.
• The first reported death was a 61-year-old male, with a long history of smoking, who succumbed to acute respiratory distress, heart failure and cardiac arrest.
• Early, unpublished first-hand reports suggest at least some patients develop myocarditis.
COVID-19 Very Similar to MERS and SARS
COVID-19 is a betacoronavirus, like severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), and presenting as viral pneumonia with a wide range of acuity, the bulletin states. As of Feb. 12, COVID-19 appears to have greater infectivity rate, but a lower case fatality rate, when compared to SARS and MERS. The ACC noted 99 percent of all coronavirus cases are in mainland China, where despite aggressive containment efforts, case counts continue to rise rapidly. Get up-to-date daily statistics from the World Health Organization (WHO) COVID-19 situation reports.
Additional 2019-nCoV Information Available in the ACC Bulletin
The ACC said 2019-nCoV is a fast-moving epidemic with an uncertain clinical profile and providers should be prepared for guidance to shift as more information becomes available. The ACC said it will be updating the bulletin as appropriate. In addition, ACC has reached out to its partners and colleagues in China expressing its support as they work to address the growing epidemic.
The bulletin includes sections covering:
• Clinical guidance given current COVID-19 uncertainty;
• Potential cardiac implications from analog viral respiratory pandemics;
• Early cardiac implications from case reports on Wuhan Coronavirus; and
• Background on Coronavirus epidemic.
The bulletin was reviewed and approved by the ACC Science and Quality Oversight Committee.
CDC Delaying Spread to U.S. But Says it is Coming
The Centers for Disease Control and Prevention (CDC) said at a Feb. 21 press conference it is working to contain the spread of the novel coronavirus (COVID-19) into the United States, but said it is unlikely to do so. The agency said it hopes to slow the spread of the virus to enable more time for the U.S. healthcare system to prepare for its arrival.
“We never expected we’d catch every traveler with novel coronavirus from China. It would be impossible,” said Nancy Messonnier, M.D., the director for the National Center for Immunization and Respiratory Diseases. “We’re not seeing spread here in the United States yet, but it is possible, even likely, that it may eventually happen. Our goal continues to be slowing the introduction of the virus into the U.S. This buys us more time to prepare our communities for more cases and possibly sustained spread.”
She said this new virus represents a tremendous public health threat. “We don’t yet have a vaccine for this novel virus, nor do we have a medicine to treat it specifically. We are taking and will continue to take aggressive action to reduce the impact of this virus, and that it will have on the communities in the U.S.,” Messonnier said.
Seasonal Flu vs. Coronavirus Infection and Mortality Rates
As of Feb. 19, the World Health Organization reported 75,204 confirmed cases of coronavirus worldwide. Only 924 of these cases are reported outside China in 25 countries. There have been 2,006 COVID-19 deaths. All but three of these were in China. Reports show the death rate is about 2.3 percent.[4]
A single center study of 138 patients diagnosed with COVID-19 in Wuhan, China, said 26 percent of patients required admission to the intensive care unit and 4.3 percent died. The study also said presumed human-to-human hospital-associated transmission of SARS-CoV-2 was suspected in 41 percent of patients.[3]
Another study published Feb. 20 for 121 symptomatic patients infected with coronavirus said about 20 percent of cases are severe and mortality is approximately 3 percent.[5]
For comparison with seasonal flu in the United States, Centers for Disease Control and Prevention (CDC) estimates that so far this season there have been at least 26 million flu illnesses. The CDC said there have been about 250,000 hospitalizations and 14,000 deaths so far from flu. The CDC said the percentage of deaths attributed to pneumonia and influenza is 6.8 percent, which the CDC said is below the epidemic threshold of 7.3 percent.[6]
UPDATED INFORMATION from April 22, 2020: COVID-19 (SARS-CoV-2) cases reported are as follows:
• 2,593,129 worldwide diagnosed cases
• 827,038 diagnosed cases in the U.S.
• 45,525 U.S. deaths
• Mortality rate range for U.S cases between 2-7.5 percent, but are consistently between 6-10 percent in patients with various comorbitities
• The CDC reported April 16, 2020, 18.8% of all deaths occurring during the week ending April 11, 2020 (week 15) were due to pneumonia, influenza or COVID-19 (PIC). This percentage is above the epidemic threshold of 7.0% for week 15 and has been increasing sharply since the end of February.