Differential diagnostics in dermatoscopy
Modern dermatoscopes allow practitioners to switch between polarised and non-polarised light modes. The two types of illumination visualise different skin structures, while conventional contact dermatoscopy, i.e. with non-polarised light, is better for showing superficial structures (the superficial epidermis to the dermoepidermal junction zone), polarised light is better for identifying deeper structures, e.g. at the level of the dermoepidermal junction (DEJ) zone or the upper dermis.
Non-polarised contact dermatoscopy requires ‘coupling’ using a liquid. This greatly reduces scattered radiation when the contact plate is resting on the skin and produces a clear, low-reflection image.
There is no need to apply oil to the skin when examining with polarised light, since a polarisation filter is used in this situation. The use of both modes in modern ‘hybrid’ instruments is often helpful in differentially diagnosing a variety of diseases. This is because in dermatoscopy, light is shed on various pieces of complementary information with both non-polarised and polarised light.
Dermatoscopy with polarised light
In polarised mode, the light reflected (polarised) on the surface of the skin is blocked out by a polarisation filter.
Examination in polarised illumination mode enriches conventional non-polarised contact dermatoscopy by providing further information – depending on the issue. Subject to the position in the skin, some structures can be better identified with polarisation, while others are easier recognised without polarisation.
- The superficial whitish structures of an orthokeratosis or the blue-white structures in a malignant melanoma’s regression zone are often presented more accurately in non-polarised mode. In contrast, crystalline structures and rosette-shaped structures in the skin lesions can be observed better in polarised mode as what are known as ‘shiny white structures’, which are associated with more collagen and are thus localised deeper. This is also frequently the case when diagnosing basal cell carcinomas. What is known as the ‘blink sign’ can be helpful here.
- In pigmented lesions with melanin at the dermoepidermal junction zone or in the dermis (junctional or blue naevi), somewhat darker shades of black and brown tones and occasionally greater variability in the pigment pattern are often observed in polarised mode.
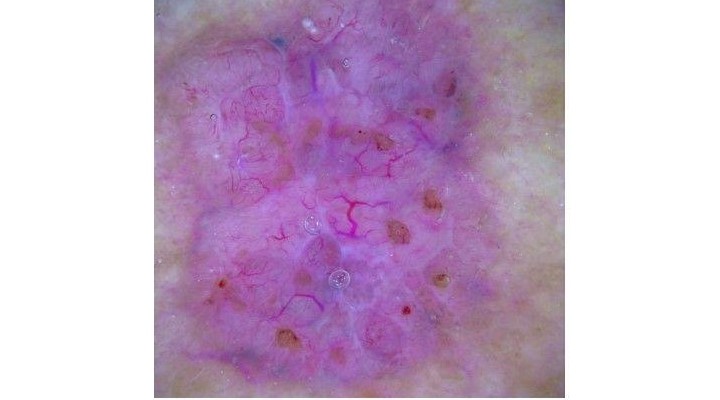
- Vascular patterns and vascular redness are also frequently more clearly recognisable with polarisation, since the vessels lie in the dermis and can be examined without any pressure effect. This can be helpful in diagnosing amelanotic or low-structure melanomas.
- In contrast, horn pseudocysts or pseudo-follicular cavities in seborrheic keratosis can become more prominent without polarisation.
Switching from polarised to non-polarised light
Quickly switching between polarised and non-polarised illumination helps with differentiated assessment and diagnosis. For example, when using the HEINE DELTA 30 or DELTAone, the toggle button can be used to conveniently switch from one mode to the other. There is no need to change the contact plate. Polarisation illumination is automatically available when the instrument is switched on.
This video shows the ‘blink sign’ when viewing a basal cell carcinoma that becomes visible when switching from non-polarised to polarised light.
When using HEINE DELTA dermatoscopes for example, you may conveniently alternate between polarised and non-polarised views with the press of a button (toggle function) – no exchange of contact plates is necessary.







-160x160-state_article-rel-cat.png)




























