Automated External Defibrillators in Basic Life Support (BLS)
This guideline is applicable to adults and children.
Background
The importance of defibrillation has been well established as part of overall resuscitation, along with effective CPR. AEDs must only be used for victims who are unresponsive and not breathing normally. CPR must be continued until the AED is turned on and pads attached. The rescuer should then follow the AED prompts.
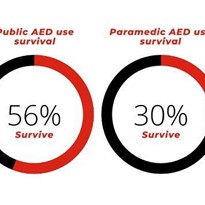
The time to defibrillation is a key factor that influences survival. For every minute defibrillation is delayed, there is approximately 10% reduction in survival if the victim is in cardiac arrest due to VF. 1
The development of Automated External Defibrillators (AEDs) has made defibrillation part of basic life support. AEDs can accurately identify the cardiac rhythm as “shockable” or “non shockable”.
Use of AED
AED use should not be restricted to trained personnel. Allowing the use of AEDs by individuals without prior formal training can be beneficial and may be life saving. Since even brief training improves performance, (e.g. speed of use, correct pad placement) it is recommended that training in the use of AEDs (as a part of BLS) be provided. 2 [Class A; LOE II, III-1, III-2, IV, extrapolated evidence]
The use of AEDs by trained lay and professional responders is recommended to increase survival rates in victims with cardiac arrest. 2 Implementation of AED programs in public settings should be based on evidence of effectiveness in similar settings.
Because population (e.g. rates of witnessed arrest) and program (e.g. response time) characteristics affect survival, when implementing an AED program, community and program leaders should consider factors such as location, development of a team with a responsibility for monitoring and maintaining the devices, training and retraining programs for those who are likely to use the AED, coordination with the local Emergency Services, and identification of a group of paid or volunteer individuals who are committed to using the AED for victims of arrest.2 [Class A; LOE I, II, III-1, III-2, III-3, IV]
Deployment of home AED’s for high-risk individuals who do not have an ICD (implantable cardioverter defibrillator), is safe and feasible and may be considered on an individual basis, but has not been shown to change overall survival rates. 2 [Class A; LOE 2, 3] Use of AED’s in public settings (airports, casinos, sports facilities, etc.) where witnessed cardiac arrest is likely to occur can be useful if an effective response plan is in place. 2 An AED can and should be used on pregnant victims.
Use of AED’s is reasonable to facilitate early defibrillation in hospitals. 2 Studies to date have shown AED’s are effective in decreasing the time to first defibrillation during in-hospital cardiac arrest. 2
Pad Placement - Adults:
Place pads on the exposed chest in an anterior-lateral position. Acceptable alternative positions are the anterior-posterior and apex-posterior. In large-breasted individuals it is reasonable to place the left electrode pad lateral to or underneath the left breast, avoiding breast tissue. All pads have a diagram on the outer covering demonstrating the area suitable for pad placement.
1 [Class A; LOE extrapolated evidence] Pad to skin contact is important for successful defibrillation. There may be a need to remove moisture or excessive chest hair prior to the application of pads but emphasis must be on minimizing delays in shock delivery.1 [Class A; LOE expert consensus opinion]
Avoid placing pads over implantable devices. If there is an implantable medical device the defibrillator pad should be placed at least 8cm from the device.1 Do not place AED electrode pads directly on top of a medication patch because the patch may block delivery of energy from the electrode pad to the heart and may cause small burns to the skin. Remove medication patches and wipe the area before attaching the electrode pad.1
Pad Placement - Children:
Standard adult AEDs and pads are suitable for use in children older than 8 years. Ideally, for children between 1 and 8 years paediatric pads and an AED with a paediatric capability should be used. These pads also are placed as per the adult and the pads come with a diagram of where on the chest they should be placed.3
If the AED does not have a paediatric mode or paediatric pads then the standard adult AED and pads can be used.2 Ensure the pads do not touch each other on the child’s chest.
3 Apply the pad firmly to the bare chest in the anterior lateral as shown above in adults. If the pads are too large and there is a danger of charge arcing, use the front-back position (antero-posterior): one pad placed on the upper back (between the shoulder blades) and the pad on the front of the chest, if possible slightly to the left4
Defibrillation Safety:
Rescuers should follow the prompts: care should be taken not to touch the victim during shock delivery. There are no reports of harm to rescuers from attempting defibrillation in wet environments.2 [Class A; LOE extrapolated evidence] In the presence of oxygen, there are no case reports of fires caused by sparking when shocks were delivered using adhesive pads.2 [Class A; LOE extrapolated evidence]
References:
1. Sunde K, Jacobs I, Deakin CD, Hazinski MF, Kerber RE, Koster RW, Morrison LJ, Nolan JP, Sayre MR. Part 6: Defibrillation: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2010; 81: e71-e85.
2. Soar J, Mancini ME, Bhanji F, Billi JE, Dennett J, Finn J, Ma MHM, Perkins GD, Rodgers DL, Hazinski MF, Jacobs I, Morley PT, on behalf of the Education; Implementation and Teams Chapter Collaborators. Part 12: Education, implementation, and teams: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2010; 81: e288-e330.
3. de Caen AR, Kleinman ME, Chameides L, Atkins DL, Berg RA, Berg MD, Bhanji F, Biarent D, Bingham R, Coovadia AH, Hazinski MF, Hickey RW, Nadkarni VM, Reis AG, Rodriguez-Nunez A, Tibballs J, Zaritsky AL, Zideman D, Nolan J. Part 10: Paediatric basic and advanced life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2010; 81: e213-e259.
4. Biarent D, Bingham R, Eich C, López-Herce J, Maconochie I, Rodríguez-Núñez A, Rajka T, Zideman D. European Resuscitation Council Guidelines for Resuscitation 2010 Section 6. Paediatric life support. Resuscitation 2010; 81: 1364-1388.



























-205x205.jpg)
